Summary: The development of an unborn child’s brain can be hampered by womb inflammation, according to researchers.
The review uncovers that over the top aggravation can prompt decreased neuronal electrical action, perhaps bringing about conditions like cerebral paralysis or formative issues influencing development, development, vision, and hearing. Additionally, this study demonstrates that electroencephalography can be used to detect these disruptions in the maturation of nerve cells.
The team stresses the significance of ensuring a healthy environment for fetuses’ optimal brain development.
Important Information:
Nerve cell maturation can be slowed down by excessive inflammation in the womb, resulting in decreased electrical activity and affecting a baby’s brain development.
This condition has the potential to cause a variety of developmental issues in infants, particularly those born prematurely, such as cerebral palsy, emotional issues, language and cognitive delays, and other issues.
Electroencephalography is a common clinical tool that can be used to find impairments in the maturation of nerve cells caused by inflammation.
Source: Hudson Institute of Medical Research It has long been known that an excessive amount of inflammation in the womb can harm the brain development of an unborn child, but how exactly this occurs has remained a mystery up until this point.
At the Hudson Institute of Medical Research, Dr. Rob Galinsky and his team concentrate on comprehending the cellular and physiological processes that hinder the development and function of the brain in the fetus and newborn.
Their most recent examination, distributed in the Diary of Neuroinflammation, shows interestingly the way in which aggravation changes nerve cell development and capability.
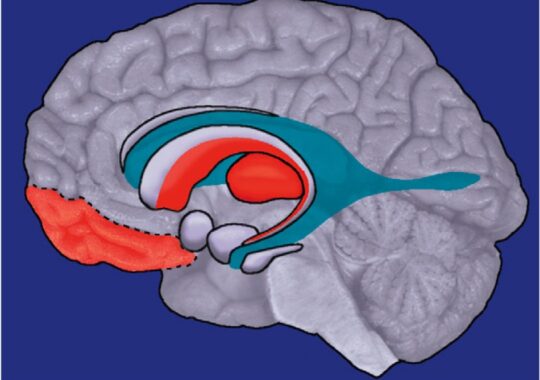
They demonstrated that excessive inflammation in the womb hinders the maturation of nerve cells, also known as neurons, which results in decreased electric activity.
Neurons are the cells in our brain and spinal cord that receive and transmit electrical signals that direct our movement, perception, perception, and cognition.
Their findings, according to lead researcher Sharmony Kelly, will help prevent or reduce a wide range of conditions that can affect babies, particularly those born preterm.
Kelly stated, “Inflammation can cause cerebral palsy or developmental problems that affect growth, movement, vision, and hearing, as well as social and emotional issues, language and cognitive delays and more.”
“We hope to assist in preventing these long-lasting consequences by increasing our understanding of exactly how inflammation damages brain development.”
According to Dr. Galinsky, “We also showed that these impairments in nerve cell maturation can be detected using a relatively simple and widely used clinical tool that measures electrical activity in the brain,” which is known as electroencephalography.
Brain development’s delicate balance “By improving our understanding of the cellular mechanisms that contribute to inflammation-induced disturbances in brain development, and their functional consequences, we can improve our ability to detect neurodevelopmental impairments earlier.”
Sharmony Kelly compared inflammation to a disruption in the development of the brain’s symphony.
“Think of the brain as an orchestra playing a tune about growth and connectivity; Like an out-of-tune instrument, the orchestra’s performance is distorted when it is exposed to inflammation.
“If the delicate balance of brain activity, cellular growth, and immune responses is upset, which could have long-lasting effects,”
“We’re causing to notice the meaning of keeping an amicable climate for solid mental health and the potential outcomes when that equilibrium is disturbed,” she said.
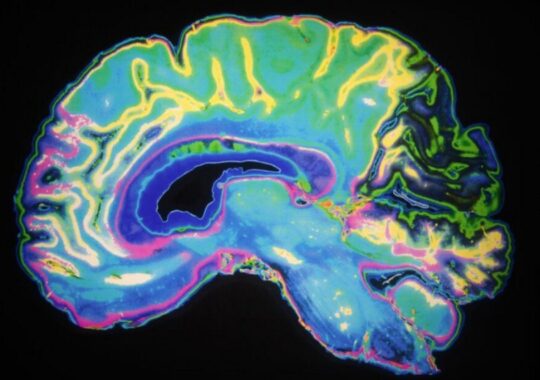
Background: Neuronal connectivity problems, slowed growth of the cortex, and poor neurodevelopmental outcomes are all linked to infection or inflammation during pregnancy. It is unclear what pathophysiological substrate underlies these changes. Electroencephalogram band power analysis was used to test our hypothesis that cortical neuronal microstructure and neural function would be altered by progressive inflammation in late-gestation fetal sheep.
Methods Fetal sheep (0.85 weeks of gestation) were surgically instrumented for continuous EEG recording and randomly assigned to repeated saline (control; n = 9) or LPS (300, 600, and 1200 ng after 24 hours, respectively; infusions to cause inflammation (n = 8). In order to examine inflammatory gene expression, histopathology, and neuronal dendritic morphology in the somatosensory cortex, sheep were put down four days after the initial LPS infusion.
Results (P 0.05 vs. control): LPS infusions increased delta power between 8 and 50 h and decreased beta power between 18 and 96 h. In the somatosensory cortex, basal dendritic length, the number of dendritic terminals, dendritic arborization, and dendritic spines were all reduced in LPS-exposed fetuses (P 0.05 compared to control). Microglia numbers and IL-1 immunoreactivity were both higher in LPS-exposed fetuses than in controls (P 0.05). The total number of cortical NeuN + neurons and cortical area did not differ between the groups.
Conclusions Despite the normal number of neurons, exposure to antenatal infection or inflammation was associated with impaired dendritic arborisation, loss of high-frequency EEG activity, and this may have contributed to disturbed cortical development and connectivity.
Disclaimer: The views, suggestions, and opinions expressed here are the sole responsibility of the experts. No Clear Insight Research journalist was involved in the writing and production of this article.